The future lies in the stem cell
“Physician researchers have reintroduced repaired cells in two young patients. Their condition both improved” - Christine Mummery, Professor of Developmental Biology LUMC
How do you repair a damaged or malfunctioning body part? That is what regenerative medicine is concerned with. Central to this today are stem cells.
Stem cells can be taken from organs or tissues, or created by so-called "reprogramming." They are capable of making new body cells; some stem cells make one type of cell, while others can make several types. “For instance, we can reprogram a skin cell into a stem cell, from which we can then create pancreatic cells.”, said Christine Mummery, Professor of Developmental Biology at Leiden University Medical Center (LUMC) and a leading figure in developing human models for drug discovery.

Mummery: “From a stem cell we can create a cell that is missing or non-functional in the body. With this, we repair tissue. Additionally, based on stem cell models, we can determine whether a drug will be effective for patients. This is called personalized medicine. All of this falls under regenerative medicine. Within the LUMC, we conduct research with these stem cells to cure various diseases in the future.”
Testing for America
For example, Professor of Diabetology at LUMC Eelco de Koning is researching how to treat severe forms of diabetes. This can be achieved by repairing a pancreas. For the past twenty years, LUMC has been transplanting insulin-producing cells from the pancreas into patients.
“Doctors at LUMC use cells from donor pancreas, not stem cells,” Mummery said. “However, there are few donors, so we can only help about eight patients a year. That’s not enough progress, which is why we want to adopt the use of stem cells that we can create in the lab. If successful, we would have a daily supply of as many cells as needed. In Leiden, we have made significant progress in this regard. To the extent that American scientists are reaching out to us for help with cell transplantation in patients.”
Cells travel, the child does not
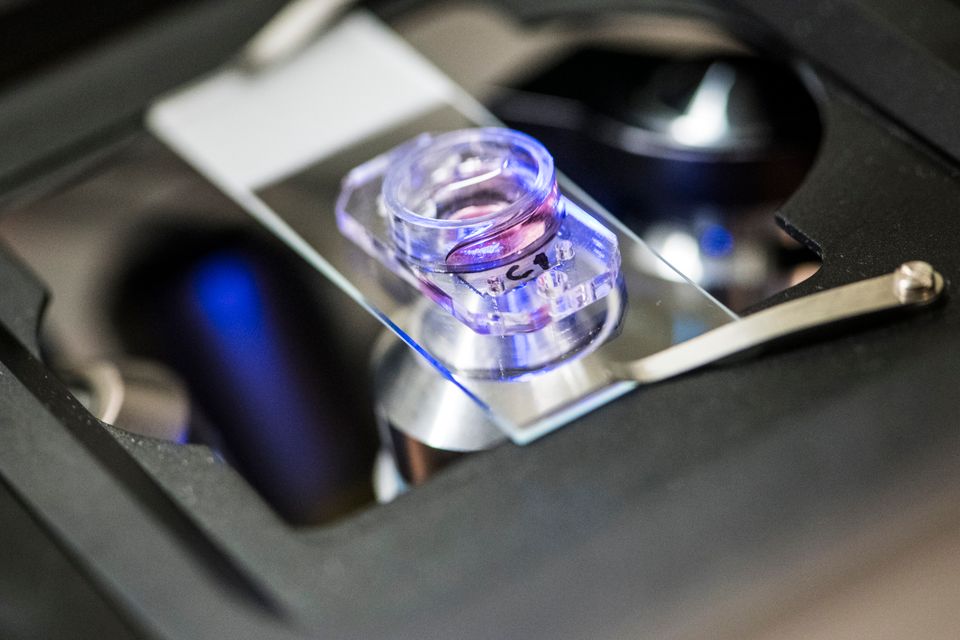
“Children with severe congenital immune disorders are reliant on stem cell transplantation treatment with stem cells from a healthy donor. Unfortunately, suitable donors are not always available. Therefore, researchers at LUMC have developed an innovative therapy where diseased stem cells from the patient's bone marrow are repaired using gene therapy and then reintroduced to the patient. Thus, the patient is actually their own donor. Two young babies have already been treated with this method, and the results are promising.”
She is enthusiastic about this European achievement, which originated from Frank Staal, Professor of Molecular Stem Cell Biology, and Arjan Lankester, Professor of Pediatrics and Stem Cell Transplantation, along with their teams. Mummery stated, "This is currently being tested in collaboration with various children's hospitals in Europe and Melbourne. The patient's stem cells are brought to LUMC, repaired here and returned to the patient as "medicine." That means the cells travel, and the child does not.”
Screening with Disease Models
Which drugs are effective and which are not? Answering this question can be challenging, especially when one disease can arise from various causes.
'We are almost at a point where we can say this for heart arrhythmias. For example, if we create stem cells from a patient with a genetic mutation, those stem cells will also carry the mutation. We generate heart cells from these stem cells and then test thirty thousand compounds to see which one corrects the mutation. That means the heart arrhythmia disappears. Presently, we possess stem cell models for various heart arrhythmias, revealing which medications are effective for specific patients,’ explains Mummery. 'We call this precision medicine; and it is an area where we excel.’

Predicting side effects
“In addition, some drugs have unpleasant side effects and can make a person ill. If someone has been cured of cancer, it is possible that ten years of chemotherapy will cause heart problems. Heart transplantation is then the only solution. Under the leadership of Sjaak Neefjes, Professor of Chemical Immunology at LUMC, variants of a cancer-inhibiting drug have been developed that have no effect on the heart yet still kill the tumor. Our heart models made from stem cells have contributed to proving the safety of these new drug variants. Neefjes and his team hope to help the first patients with this new drug as early as January 2024. A milestone for Leiden.”